A case study: chronic haemodialysis
Presentation of the technique
Chronic kidney disease (CKD) is a common and serious illness which, in its terminal phase, carries a high risk of death. Management of end-stage renal disease most often involves supplementary treatment, dialysis or kidney transplantation. Haemodialysis is the most widely used treatment technique, involving more than 90% of dialysis patients (49,000 patients in France, nearly 3 million worldwide).
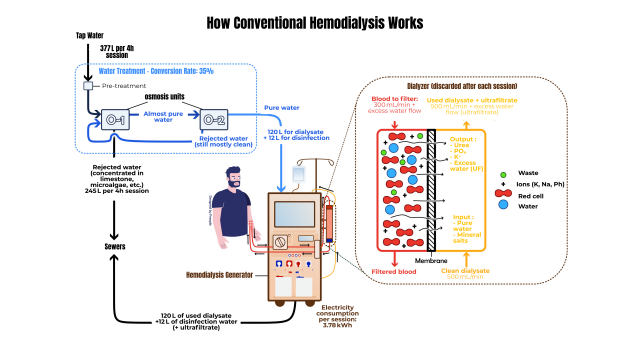
This technique involves filtering the blood through a dialysis membrane (dialyser or artificial kidney) using an extracorporeal circulation system, then returning it to the patient. The toxic substances to be purified are transferred through the semi-permeable membrane from the blood to a specific liquid called dialysate. The deployment of haemodialysis requires a large amount of medical equipment and consumables: water treatment (to produce the ultrapure water that makes up 97% of the dialysate), a dialysis machine (which produces the dialysate continuously and generates fluid circulation via a system of pumps), and specific single-use medical devices (which enable the extracorporeal circuit to be reconstituted, provide filtration or are used in the composition of the dialysate). Sessions last around four hours and are generally repeated three times a week.
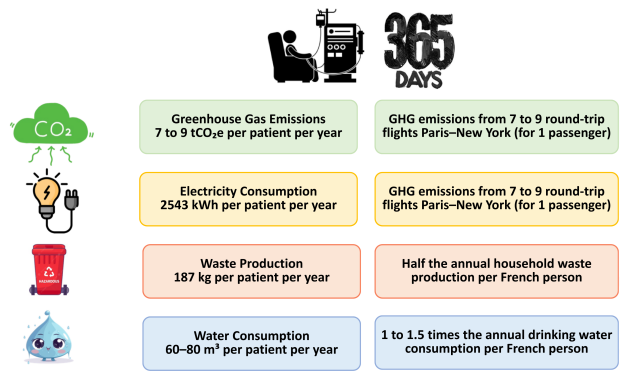
Although vital for patients, haemodialysis is also associated with significant consumption of resources and a major environmental footprint, as illustrated in the figure below.
In this context, and in view of the continuing increase in the number of patients with chronic end-stage renal disease, it is crucial to transform our practices towards greater sustainability.
The aim of the rest of this chapter is to explore case studies based on haemodialysis, in order to illustrate how it is possible to put in place a process for assessing and reducing the environmental footprint of a healthcare practice.
Carbon footprint for haemodialysis centres
Justification for the study
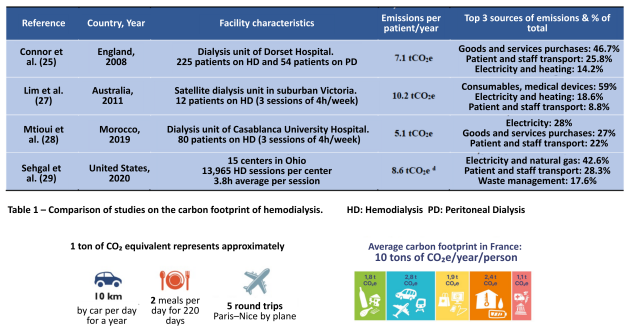
A few studies have attempted to quantify the carbon footprint of conventional haemodialysis by including all the direct and indirect emissions associated with the treatment activity. In 2010, one of the first publications by a British team reported an annual carbon footprint of 7.1tCO2e per patient (Connor et al). Subsequent studies published by Australian and American teams found comparable results, with annual carbon footprints of between 8.5 and 10.5 tCO2e per patient (Lim et al, Sehgal et al). The data suggests that the largest contribution to emissions comes from pharmaceuticals and medical devices, energy consumption in buildings, and patient and staff travel.
However, the data currently available in the literature has a number of limitations that make it difficult to extrapolate it to the French context in order to develop a relevant decarbonisation strategy. These limitations include the use of emission factors derived from national registers for the majority of activity data, and the use of a monetary emission factor for medicines, medical devices and equipment (in the absence of specific life cycle analyses).
It was against this backdrop that research was carried out to produce a BEGES for haemodialysis centres in France, using the Bilan Carbone approach developed by ADEME and the Bilan Carbone association (a reference standard compatible with other international protocols).
Scope of the study
A total of 19 centres were included as partners in this study, with the aim of providing a sample that illustrates the diversity of care provision in the region. The centres vary in terms of the sector to which they belong (public, not-for-profit and private), the type of care offered (heavy centre, medicalised dialysis unit, self-dialysis unit1), the area in which they are located (urban, suburban, rural) and their size. All these factors have a decisive role to play in the way care is organised, and therefore possibly in the profile of greenhouse gas emissions.
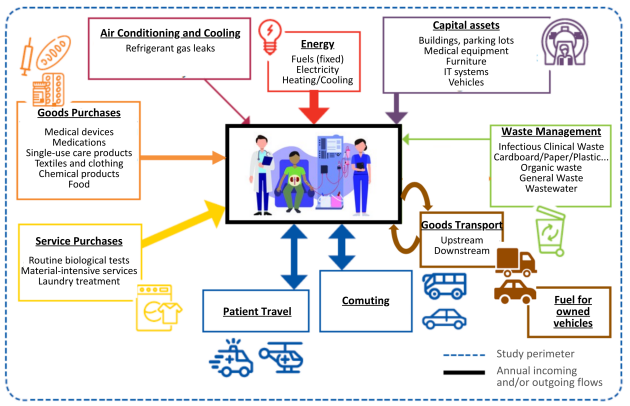
Operational scope of the study
The first phase was to optimise the methodology so that it met the constraints encountered in this activity. Preliminary work based on a review of the literature, consultation with engineers specialising in the BEGES and interviews with medical-technical teams enabled the methodology to be transposed in order to adapt it as closely as possible to the specific characteristics of haemodialysis. Thirteen emission items were selected as relevant to haemodialysis activity, from the 22 that exist in the official nomenclature. The figure below shows the detailed mapping of emission sources as included in this work. The reporting period is 2022 (from 01/01/2022 to 31/12/2022).
Data collection method and emissions factors used
All the data used to produce the BEGES is primary data specific to the establishment. This data was collected with the help of the teams at each centre from existing monitoring registers, data extraction from management or pharmacy software, or field surveys carried out specifically for the BEGES.
Most of the emission factors were taken from La Base Empreinte® (the official public database of emission factors administered by ADEME). For medicines, medical devices, medical equipment and chemicals, a monetary ratio has been used until specific life cycle analyses are available.
Results of the study and discussion
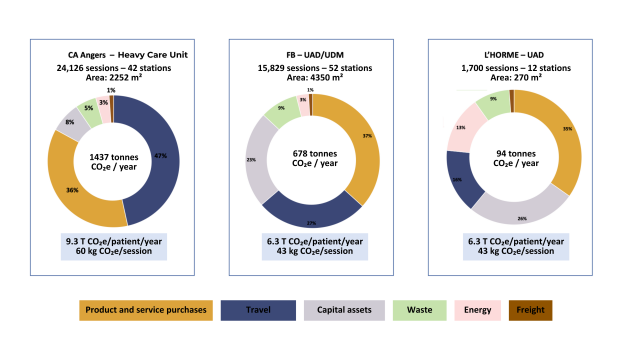
Across the 19 centres, our results confirm the significant carbon footprint associated with in-centre haemodialysis:
Between 5.6 and 14 tCO2e per patient per year (based on 3 sessions per week) with an average of 7.5 tCO2e (± 1.8)
Between 36 and 90 kg CO2e per session, with an average of 48.5 kgCO2e (± 11.6)
Emissions are mainly indirect. The three largest emitters are :
Purchases of products and services (dominated by medical devices and medicines), which systematically account for at least a third of total emissions.
Travel, dominated by patient journeys (almost all of which are made in private vehicles)
Fixed assets (dominated by dialysis medical equipment and/or buildings)
Energy (whose major share of emissions is linked to the use of natural gas for heating) and waste treatment still account for less than 10% of emissions. Finally, freight, when assessed, is a minority item at around 2 to 5%.
The disparities between the centres (both in terms of overall BEGES and the breakdown between emission items) can potentially be explained by: the intensity of the care required by heavy-care centres, the geographical proximity between the centre and the patients' homes, the operating mode of the facilities (opening hours and number of rounds per day), the centre's occupancy rate and the size of the building. In addition, the variability of the data available and the uncertainty surrounding their collection may introduce methodological biases, which must be taken into account when analysing the results.
The figure below shows the breakdown of emissions by category and by item for 3 centres with very different profiles in terms of size, care methods and geographical location.
The BEGES: a decision-making tool for decarbonisation
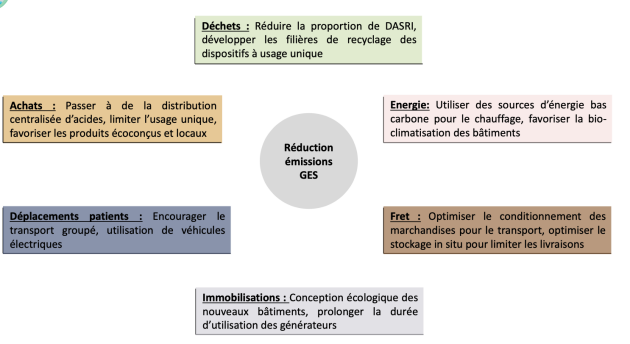
Once the BEGES has been produced, it must be used as a decision-making tool to guide the implementation of an appropriate decarbonisation strategy based on empirical observations obtained in real life.
The measures to be adopted must be based on an approach that incorporates the point of view of each centre, in its own specific context, in order to establish a coherent roadmap based on measures relating to the highest-emission items and prioritising feasibility and acceptability imperatives.
The Société Francophone de Néprhologie Dialyse et Transplantation (SFNDT) (French-speaking society for dialysis and transplantation) has published a Guide to Good Green Dialysis Practice to guide those involved in the process. This guide sets out the levers for action in 10 key areas, with a general introduction for each, a list of actions based on the time required to implement them, focus sheets for certain emblematic actions, and a summary of sourced feedback. The guide is available as a free download from the SFNDT website (in French and English).
Lifecycle analysis of the haemodialyser
Rationale for the study
The haemodialyser (or dialysis membrane) is the central device at which exchanges take place between the blood and the dialysis fluid that will circulate on either side of the semi-permeable membrane. A new haemodialyser is needed for each session, with patients usually receiving 3 sessions a week.
Haemodialyzers are complex medical devices: they are associated with a high level of criticality due to their direct and prolonged contact with the patient's blood. They must meet stringent requirements in terms of technical performance, biocompatibility and hygiene - requirements that are regulated by a strict standards framework. In practical terms, this means that specific materials (synthetic polymers) have to be chosen, complex industrial transformation processes involving several stages have to be carried out, and products have to meet high quality standards.
To date, there is little information available on the environmental impact of haemodialyzers. Having a reliable methodology and data on life cycle analysis will have a number of interesting spin-offs:
Use a specific emissions factor in the BEGES to avoid the uncertainty associated with the monetary ratio
Describe the distribution of impacts over the entire life cycle to inform an eco-design approach for the product
Compare the environmental footprint of several haemodialyzer references to include the environmental criterion when making a choice (in addition to the clinical criteria of purification quality, biocompatibility and economic criteria) as part of an eco-prescription approach.
To provide food for thought on the relevance of reusing haemodialyzers
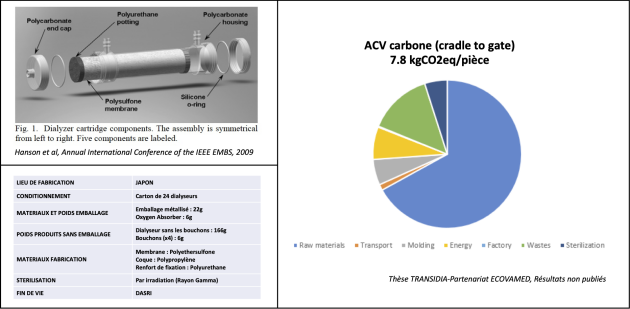
Detailed single-carbon LCA of a haemodialyser (cradle-to-gate)
The LCA approach was carried out under the direction of ECOVAMED (a company specialising in LCA of healthcare products).
The functional unit chosen was: ‘Provision of a haemodialyzer A in a dialysis department in France (cradle-to-gate approach)’. It therefore excludes end-of-life (since in the BEGES this is accounted for under a dedicated waste item).
A detailed life cycle inventory was drawn up based on the expertise of ECOVAMED's engineers, who have in-depth knowledge of the petrochemical and pharmaceutical industries combined with specific know-how in LCA of healthcare products, including models developed in-house on the environmental impact of certain specific processes such as sterilisation. The database used is ECOINVENT.
The manufacturing process was divided into several successive stages:
Extraction of raw materials
Transport n°1 upstream of the plant
Manufacturing and sterilisation process
Transport n°2 downstream from the factory to the customer for final use.
Each of these stages is constructed by combining the manufacturer's public data (materials, place of manufacture, sterilisation method), data collected empirically (weight per material), and hypotheses formulated to complete the missing data (energy consumption, industrial processes, loss of material at each stage of manufacture, infrastructure, mode of transport, etc.).
This gives a carbon footprint of 7.8kgCO2e per haemodialyser. The stages that contribute most are the extraction of raw materials, waste treatment and energy consumption. These data should be taken as an initial preliminary result, to be consolidated at a later date.
The average unit price was €7.7 per dialyser. In monetary terms, this corresponds to 1012kgCO2e/k€. However, the generic monetary ratio is 315kgCO2e/k€. This means that for a complex medical device such as a haemodialyser, the generic monetary ratio underestimates the ‘real’ carbon footprint by dividing it by a factor of 3.2. This example demonstrates the value of calculating a specific unit emission factor to avoid the uncertainty inherent in the monetary ratio.
The reuse of haemodialyzers
Despite their complex and critical nature, the re-use of haemodialyzers is a widespread practice in many countries around the world for essentially economic reasons, particularly in South America and Asia. It is also the subject of international recommendations setting out the standards and good practice to be observed.
Reuse, seen as a response to shortages, scarcity of resources, carbon impact and the high cost of medical devices, therefore seems particularly relevant here, especially given the frequency of care, the chronicity of dialysis, the increase in the number of dialysis patients, dependence on the petrochemical industry, and the associated economic and environmental costs.
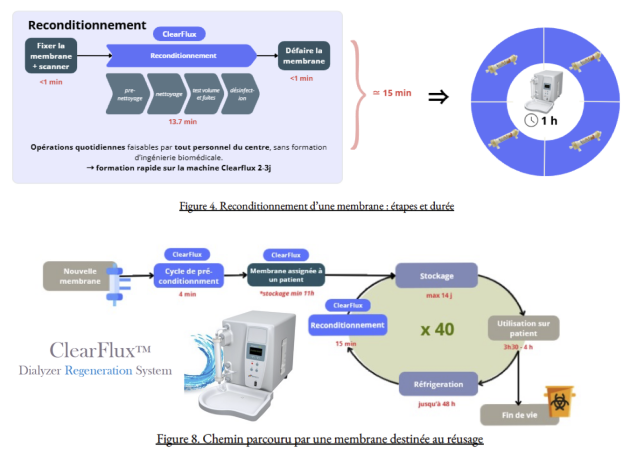
In addition, there are several technological processes and equipment that make it possible to perform reconditioning in an automated manner to limit risks to patients. One specific hemodialysis reprocessing device recently designed and marketed in the United States by Novaflux is the "ClearFluxTM Dialyzer Reprocessing System" (hereinafter referred to as Cleaflux System). The Clearflux System is a fully automated and standardized high-flow hemodialysis reprocessing equipment with a polysulfone membrane for reuse. The system also provides pre-treatment of hemodialyzers before they are assigned to patients for their first use, as well as monitoring the retired hemodialyzer for limited use to the patient to whom the hemodialysis was originally assigned. The system was approved by the Food and Drug Administration (FDA) for marketing in the United States in September 2010. The reprocessing of a hemodialysis device by the ClearFlux System includes several steps (detailed in the figure below). The cleaning phase consists of a patented two-phase process called Two-Phase Flow (liquid and gas) that completely removes biological contaminants and adherent substances (protein deposits and thrombosis). This cleaning mode allows for a quasi-adherent recovery of the hemodialysis device's properties, which can be reused up to 40x for the same patient.
However, it should be noted that at present, the reuse of hemodialyzers is prohibited in France in accordance with an ordinance of April 2022 that explicitly prohibits the reprocessing of single-use DMs. The prospect of implementing this practice in the future could be considered according to two different strategies:
Amend the national legislative framework to allow the reprocessing of UDU (i.e. allow the application of Article 17 of Regulation (EU) 2017/745 on medical devices).
Introducing reusable haemodialyzers to the European market. In this case there is no need to change the legislation. However, the initiative can only come from the manufacturers themselves, who will have to complete the steps to obtain CE marking for their devices and take on the responsibilities of manufacturers of multi-use medical devices.
Faced with this observation, a reflection is necessary in order to explore the relevance of the reuse of hemodialysis machines in France according to a transversal approach associated:
An analysis of the risk to patient safety. In its 2010 report to the European Parliament and the Council on the issue of reprocessing medical devices in the European Union, the Scientific Committee on Emerging and Emerging Health Risks (CSRSEN) identified three significant risks to patient safety that could result from a reprocessing procedure: impaired device performance, persistent chemicals used and persistent contamination.
An environmental assessment. The ecological relevance of hemodialysis reprocessing has not yet been determined and depends on multiple parameters that need to be rigorously assessed. Indeed, reuse is associated with a reduction in upstream consumable production and a decrease in the volume of solid waste downstream. Nevertheless, cleaning and repackaging processes could generate several million liters of chemical liquid waste depending on the techniques used. Hence the need for a multi-criteria environmental impact assessment based on a robust ACV-type methodology for a comprehensive assessment of the benefits and risks of dialysis reuse.
A socio-technical feasibility study. It aims to assess how the introduction of a process for the reuse of haemodialyzers within a structure will change its organisation by taking into account both technical and social aspects. It seeks to analyse whether the envisaged technological solutions are feasible and adapted to the needs of the users, while taking into account social, cultural and organisational constraints. The aim is to ensure that the project can be implemented effectively and accepted by stakeholders, while addressing technical, human and economic challenges.
An analysis of the regulatory framework. The objective here is to understand what regulatory requirements will have to be met in order for the Clearflux medical device to be placed on the European market. On the other hand, it will be to shed light on the regulatory issues related to the re-use of medical devices in order to understand the opportunities and limitations imposed by the legislation in order to ultimately attempt to draw the contours of a possible trial for longer-term clinical use.
An analysis of the economuc and financing stakes. The economuc chain needs to be partially reinvented. La chaîne économique doit être partiellement réinventée. The economic chain needs to be partially reinvented. Specifically, this involves replacing the current model based on « singke use - disposal » with a model that prioritizes « multiple use - repackaging ». From a financial perspective, this means replacing the recurring costs of purchasing and managing waste with investments in durable equipment and time spent on repackaging. Understanding how this change will affect funding mechanisms within health care facilities, as well as national policies on funding and reimbursement for care.
Consideration of ethical and responsibility considerations. The transition from single use to reusable raises ethical concerns, particularly regarding potential inequalities between patients. It is therefore crucial to address issues related to prior patient information and obtaining their informed consent. With regard to liability, it is necessary to clarify the roles and responsibilities of each actor involved (healthcare professionals, hemodialysis manufacturer, repackaging system manufacturer, natural and legal person in charge of repackaging, care facility) in particular on the issue of risk management and quality management.
LCA of the dialysis machine
Rationale for the study
The deployment of haemodialysis requires a dialysis generator (which produces the dialysate continuously and generates fluid circulation via a system of pumps). Since the technique was invented in the 1920s, generators have evolved considerably, improving the quality of care and patient safety. These technical advances are part of a process of (high)technicisation. This is essentially reflected in the design of machines of increasing complexity, incorporating more and more digital technologies and meeting the objective of continuous automation of a certain number of processes. However, to date there are no robust studies published in the literature to provide information on the environmental impact of this central piece of equipment in the healthcare process. Furthermore, it is impossible at present to estimate the additional environmental costs potentially generated by this systematic trend towards increasing the complexity of technical objects, which seems to guide research and development policies in the name of a certain idea of innovation in healthcare, technical progress and healthcare performance.
It was against this backdrop that it seemed essential to undertake this work aimed at developing a reliable and reproducible methodology for assessing the environmental footprint of generators. In particular, this was to meet two objectives:
To have a specific carbon footprint that will be included in the BEGES for haemodialysis, so as to avoid using a monetary ratio for this item.
To provide a detailed analysis of the environmental impact in order to inform the eco-design of a sustainable generator.
Description of the de la methodology
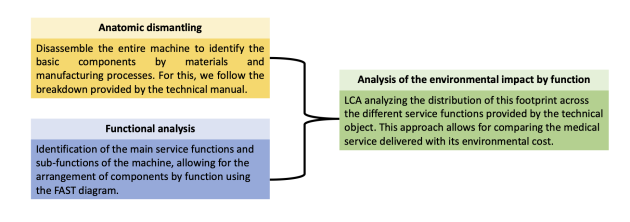
In terms of methodology, we have implemented a hybrid approach combining :
A Life Cycle Assessment to model all the impacts over the entire life cycle, from the extraction of raw materials, through all the activities involved in the production and use of the product, right up to its end of life.
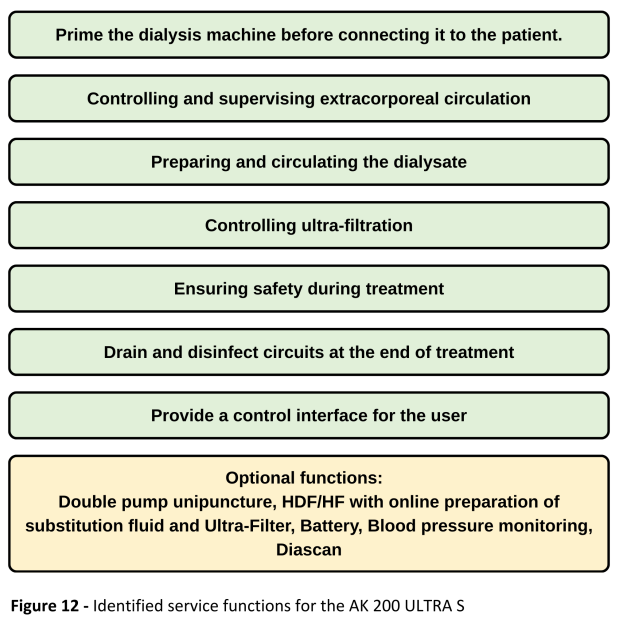
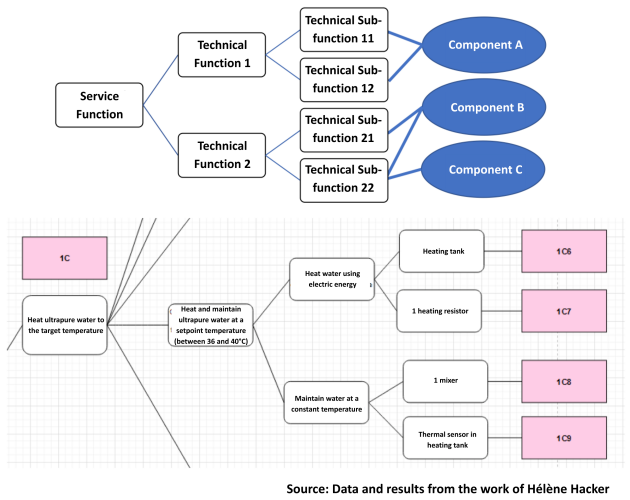
A function analysis system technique (FAST) to shed light on the link between environmental cost and medical service rendered. This analysis consists of drawing up a diagram that presents a rigorous translation of each of the ‘service functions’, i.e. the actions carried out by the product to meet an element of the user's need (in this case, ensuring extra-renal purification). Within these service functions, ‘sub-functions’ are grouped together, representing the internal solutions chosen by the product to provide the service function. Each sub-functionality is itself made up of an association of ‘components’ (the many parts that make up the equipment), which will be analysed in terms of material (type of material, weight, transformation process, etc.).
The model used here is a GAMBRO AK 200 ULTRA S generator, launched in 1995. This is an ‘old generation’ piece of equipment, production of which ceased a few years ago. This model was chosen for several reasons. Firstly, there was a model available at the UTC that could be completely dismantled. Secondly, historically, it is a model that has been widely used and which offered a good quality of care. Finally, other generators from the same manufacturer currently on the market (ARTIS PHYSIO) are based on the same design and principles.
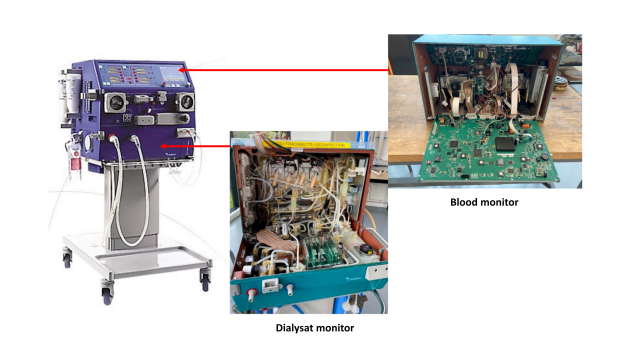
The machine consists of a dialysate monitor (in charge of manufacturing and circulating the dialysate), a blood monitor (in charge of extracorporeal circulation), a monitor support, specific components (in charge of optional haemofiltration functions), and electronic circuits.
Anatomical dismantling: examples of results
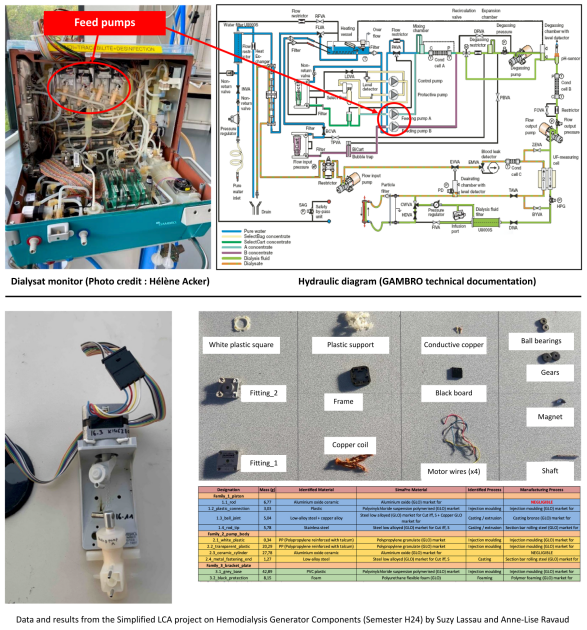
A systematic method has been put in place to dismantle and identify the components of each unit. Here are the key steps:
Locate the unit and visually identify its components.
Extract the parts, dismantle them and separate them according to the manual, distinguishing between ‘elementary parts’ (single material) and ‘complex parts’ (assemblies).
Identify the materials of the elementary parts, group them by material and weigh each assembly.
For complex parts, break them down into elementary parts, taking into account the different existing references.
Record the inventory in a spreadsheet, which will be used as the basis for the environmental analysis in the SIMAPRO software.
The figures below illustrate the example of a complex part of the dialysate monitor: the feed pumps, whose function is to dose a precise volume of concentrate used in the manufacture of the dialysate. Each pump consists of a stepper motor and a ceramic piston pump. The results presented come from work carried out by two UTC students as part of a TX.
Functional breakdown: initial results
In order to produce the FAST diagram, it is first necessary to establish exhaustively the service functions that contribute to ensuring extra-renal purification. It then requires a precise understanding of the design of this specific equipment in order to identify the various sub-functions chosen by the designers. The final step is to link the components (which are in fact the elementary and complex parts catalogued by the inventory of the anatomical disassembly phase) to each of these sub-functions.
The data contained in the manufacturer's technical documentation, and in particular the flow diagrams for the dialysate monitor and the blood monitor, were used in addition to an interview with a biomedical engineer who has in-depth knowledge of this model.
One of the difficulties here will be to be able to put in place relevant allocation rules for multi-functional components, support components and electrical consumption during the use phase.
The figures below illustrate the service functions identified for the AK-200 as well as an example of functional breakdown (FAST sub-section). The results come from work carried out by a UTC student as part of a TX.
Expected final results and outlook
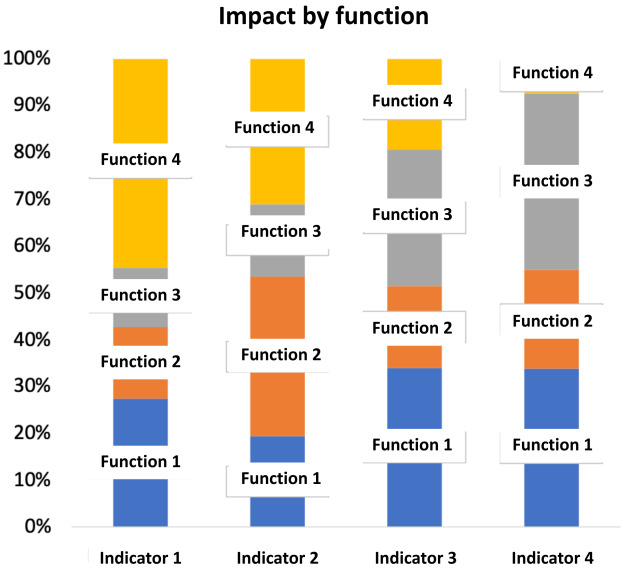
Once the process has been completed, we will have an analysis of the environmental impact by functionality over the entire life cycle of the object. By including the life cycle analysis in the analysis of the machine's functionalities, it will be possible to take a critical look at the various functions of the generator and compare the medical service rendered with the environmental cost.
The consolidated results of this hybrid approach for the AK200 could therefore serve as a basis for the subsequent study of ‘new generation’ models. Comparing the functional LCAs of several machines (old versus new generation) would appear to be a good approach for analysing the dynamics of high (technicisation) at work and their ecological implications.
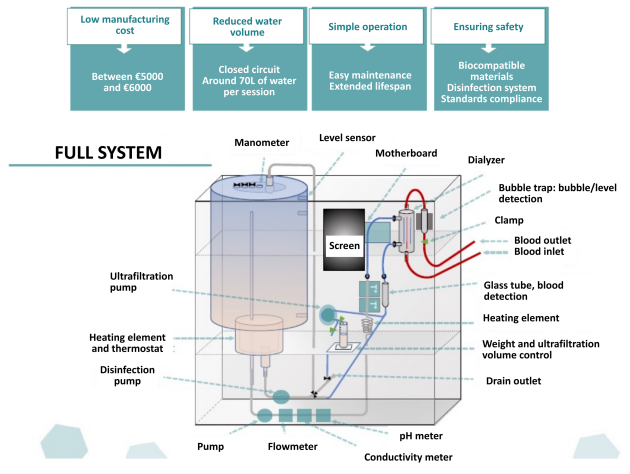
Finally, the aim is also to provide empirical elements to shed light on an eco-design approach for a dialysis machine aimed at integrating environmental requirements in terms of increasing scarcity of material resources, reducing the ecological footprint, robustness and equity of access to care in a world constrained by exceeding planetary limits. Against this backdrop, the question arises as to the place of low-tech in healthcare as a possible response to the global health challenges of the Anthropocene. Reflections are already underway on this subject, as illustrated by the prototype diagram presented below, based on the work of a Franco-Vietnamese nephrologist, Pr Mann, and taken up and consolidated by UTC students as part of a TX.