Assessing environmental impact: an essential prerequisite
Environmental reporting in healthcare: what's at stake?
Healthcare establishments and facilities are currently faced with competing priorities at a time when they are already engaged in numerous measurement and quality management processes. New environmental reporting requirements, particularly those relating to greenhouse gases, are likely to be perceived as restrictive. However, the urgency of the climate crisis and its implications for public health and the preparation of healthcare systems make such efforts necessary. The decarbonisation of healthcare activities can be seen as an additional dimension of quality of care, given that the pollution generated by the healthcare sector can harm patients, healthcare workers and society in general.
In this context, indicators make it possible to report on performance and ensure transparency, with a view to accountability. Similarly, measurement can help to inform local improvement efforts by healthcare facilities and organisations, assess and facilitate the sharing of decarbonisation initiatives, and identify best practice.
Additional indicators specific to the healthcare sector will be needed to define and establish benchmarks for progress and serve as key indicators of decarbonisation performance. It is also necessary to take into account standardisation factors that reflect clinical activity. Combining these measures with existing health system performance indicators (e.g. quality and efficiency of care, costs, equity and outcomes of care) can ensure that the effects of decarbonisation go hand in hand with maintaining or even improving the quality of care.
Governance and infrastructure are needed to implement greenhouse gas accounting, external performance reporting and internal data-driven strategic management. To facilitate the rapid adoption of GHG accounting, healthcare organisations will need support and guidance, particularly on the data sources to be used to generate reports. Difficulties that may be encountered by those undertaking such an approach include: the lack of data relating to the specific environmental impact of the consumables on which the healthcare system depends (drugs, medical devices, equipment), the opacity of manufacturers' data and the sensitive nature of healthcare data, and the complexity of supply chains.
Furthermore, as healthcare institutions and facilities have limited resources, they will first focus on measures explicitly required by legislation, certification and funders. Political changes concerning funding and accreditation will be necessary to support the implementation of environmental reporting processes in healthcare, paving the way for a coherent and effective decarbonisation strategy.
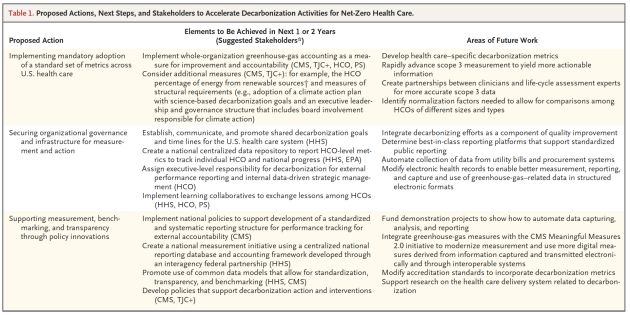
* CMS denotes Centers for Medicare and Medicaid Services and other payers, EPA Environmental Protection Agency, HCO health care delivery organization, HHS Department of Health and Human Services, PS professional societies of HCOs, and TJC+ the Joint Commission and other oversight bodies.
† This percentage will depend on factors such as location, local climate, and local grid mix.
In France, there are now a number of regulatory and governance initiatives aimed at guiding and supporting the transformation of the sector towards greater sustainability. Two of these initiatives focus on the issue of greenhouse gas emissions.
Decree no. 2022-982 of 1 July 2022 updates the regulatory provisions relating to GHG emissions assessments.
From now on, the scope of GHG emissions taken into account will be extended to include: direct emissions linked to an organisation's activity (scope 1), emissions from energy consumption (scope 2), and significant indirect emissions linked to operations, activities and the use of goods and services produced by the company (scope 3). The aim of this development is to provide companies with a more comprehensive view of their carbon footprint. Indirect emissions are identified and quantified using a precise methodology defined in article R. 229-49 of the French Environment Code. Healthcare establishments are therefore subject to the application of this law (for legal entities under public law with more than 250 employees and for legal entities under private law with more than 500 employees). The maximum penalty for failure to comply is €10,000, and €20,000 for a repeat offence.
An ecological planning roadmap for the healthcare system was published in December 2023 under the aegis of the Ministry of Health as part of the work of the steering committee set up for the healthcare sector to control its environmental impact and ensure the sector's ecological transformation over the long term. This roadmap sets out the means and measures for achieving the target objectives of contributing to carbon neutrality in the healthcare sector and controlling environmental risks. These objectives are :
Accelerating the ecological renovation and energy transformation of healthcare and medico-social establishments by 2040
Accelerate the ecological transition of healthcare industries and products
Accelerate and promote the transition to sustainable procurement by 2030
Transforming and supporting practices towards eco-responsible care by 2023
Accelerate the reduction and recovery of waste by 2030 and optimise the scope of waste from infectious risk healthcare activities (dasri) to limit it as much as possible by 2024
Train and raise awareness among all healthcare professionals and stakeholders of the ecological emergency, health-environment issues, eco-design of care and medico-social support, and support research projects between now and 2025.
Accelerate the transition to low and very low emission transport and mobility schemes by 2030
Draw up a roadmap for greening digital healthcare by 2024
The next few paragraphs of this chapter will be devoted to two tools for carrying out an environmental assessment: the Carbon Footprint and the Life Cycle Assessment (LCA).
The Carbon Footprint
Definition
The French Environment and Energy Management Agency (ADEME) defines carbon footprint as ‘an assessment of the quantity of GHG emitted (or captured) into the atmosphere over one year by the activities of an organisation or territory. The entity's emissions are ordered according to predefined categories called items’.
A carbon footprint is produced in stages :
1. Firstly, define the operational and organisational perimeter concerned by the assessment in order to map all the emission sources precisely;
2. Next, collect activity data linked directly or indirectly to the physical flows of people and materials within the defined perimeter;
3. Finally, calculate the balance sheet by applying the appropriate emissions factors to translate the physical flows into the quantities of CO2e that will finally be summed up.
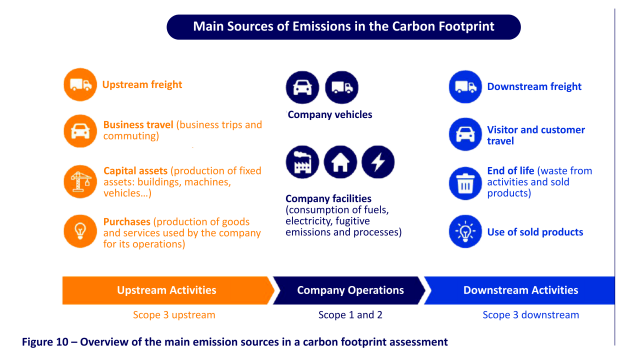
The aim is therefore to draw up a broad inventory of the GHG emissions associated with an organisation's activities, and then to sum up these emissions. For the sake of clarity, and because the levers for action are not the same, emissions are usually classified into different categories (known as ‘items’, which are themselves grouped into ‘scopes’) depending on whether they relate directly to the activity of the organisation itself, or to its upstream or downstream activities:
Scope 1: Direct greenhouse gas emissions. These are greenhouse gas emissions that occur directly within the company. Some examples: emissions linked to gas heating in an office or factory, emissions linked to fuel combustion in company-owned service vehicles, refrigerant gas leaks from air conditioning, fridges or cold rooms.
Scope 2: Indirect energy-related emissions. These are mainly emissions linked to electricity, which is not emitted directly in the workplace but when it is produced.
Scope 3: Other indirect emissions. These cover all other indirect greenhouse gas emissions, upstream and downstream, which are a consequence of the company's activities, but which are not emissions from sources owned or controlled by the company. This includes, among others, emissions associated with products bought and sold, as well as those linked to employee travel and waste management.
Several reference standards exist for GHG accounting, which can be used depending on needs and regulatory requirements: Bilan Carbone (developed by ADEME and the Bilan Carbone Association), ISO protocols (ISO 14064-1:2018, ISO 14069:2018, the GHG Protocol (developed by the World Resources Institute and the World Business Council for Sustainable Development). In France, in accordance with article R.229-48 of the Environment Code, the Ministry responsible for the Environment must publish the methodological information needed to comply with the BEGES requirements set out in article R. 229-47. ADEME has published the new version of the regulatory method on the BEGES platform to provide the guidelines for this new application, which must be applied to all GHG balances produced and published on the platform from 1 January 2023. Sector-specific guides are produced by trade associations in collaboration with ADEME, with the aim of adapting the rules and methods for estimating GHG emissions to the specific characteristics of each sector of activity. The sector guide for the healthcare sector was updated in 2020.
Concrete Applications in the Healthcare Sector
The Carbon Footprint can be used to assess GHG emissions of healthcare activities at different levels:
For a national healthcare system (as carried out by the SHIFT Project for the French healthcare system, with results presented in Part 2 of the course).
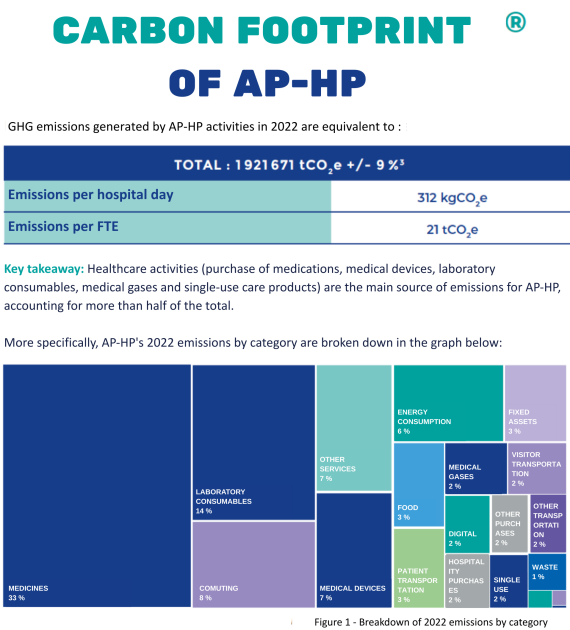
For a healthcare organization that includes one or more establishments. The example of the carbon footprint of the Assistance Publique – Hôpitaux de Paris (APHP) is detailed below.
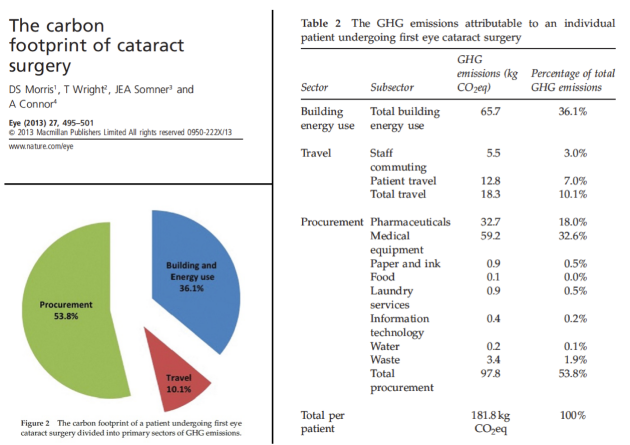
For a specific healthcare practice, such as a care pathway, a hospital stay, or a given therapeutic procedure, whether medical or surgical. The example of the carbon footprint of cataract surgery is detailed below.
AP-HP is a world-renowned university hospital center with a European dimension. It is organized into six hospital-university groupings, based around five universities in the Paris region. Every year, its 38 hospitals welcome 8.3 million patients: for consultation, emergency care, scheduled hospitalization or home hospitalization. The AP-HP is the largest employer in the Paris region, with 100,000 doctors, researchers, paramedics, administrative staff and workers.
Life Cycle Assessment
Definition
ISO 140401 defines LCA as ‘the compilation and evaluation of inputs and outputs between a production system and the environment, and their potential environmental impacts, corresponding to the life cycle of a product’.
LCA is a comprehensive, multi-criteria assessment tool that measures the quantifiable effects of products or services on the environment by identifying and quantifying the physical flows associated with their production and use.
LCA is based on two complementary approaches:
Life cycle approach: This analyses all the stages in a product's life cycle, from the extraction of raw materials to the end of the product's life (manufacture, transport, use, disposal, etc.).
Multi-criteria approach: This assesses the flows in (such as raw materials and energy) and out (such as waste or emissions) at each stage of the cycle, and their potential impact on the environment.
LCA consists of several stages:
Defining the objectives and scope of the study: The objectives of the LCA are set (comparison, eco-design) and the boundaries of the system studied are defined, as well as the functional unit (the unit of measurement that assesses the service provided by the product).
Lifecycle inventory: The incoming and outgoing flows for each phase of the product lifecycle are quantified and related to the chosen functional unit.
Environmental impact assessment: The potential impact of the flows on the environment is assessed using two types of method:
Midpoint methods: These assess impacts at an intermediate stage in the causal chain (for example, the impact on global warming measured in CO2 equivalent).
Endpoint methods: These focus on the final damage, such as the loss of biodiversity over a given area (‘Potentially Disappeared Fraction of Species’).
Interpreting the results: The results are analysed in relation to the objectives set, and areas for improvement can be identified to reduce the product's environmental impact.
This approach provides an overview of the environmental effects of a product, so that they can be better understood and reduced.
Practical applications in the healthcare sector
LCA can be used in different contexts and for different purposes in the context of healthcare:
Carrying out an LCA for a given product (medicines, medical devices or equipment) then provides a specific carbon footprint that can be incorporated into the BEGES, thereby eliminating the need to use a monetary ratio.
Propose a detailed analysis of the environmental impact of a tool or care pathway in order to inform an eco-design approach aimed at achieving greater environmental sustainability in future uses.
Compare several healthcare products offering an equivalent rendered medical service (drugs or medical devices) in order to take into account the environmental criterion at the time of the care act (diagnostic or therapeutic).
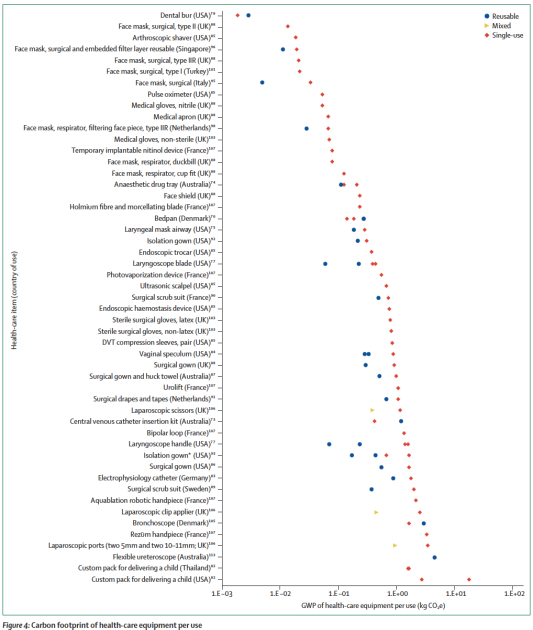
For example, the figure below shows the results of studies published in the literature assessing the carbon footprint of healthcare equipment according to its use (reusable, mixed, single-use). It shows that this carbon footprint can range from a few grams to several tens of kgCO2e per device. For single-use instruments, the carbon footprint comes mainly from the production process, while for reusable instruments, it comes mainly from the impact of the washing and sterilisation processes.
Each data point constitutes an individual carbon footprint estimate for a specified item. Reusable (blue circle), single-use (red diamond), and mixed items (yellow triangle). Mixed refers to equipment that is predominantly reusable, but which contains single-use components. Impact estimates are plotted with a log scale. GWP=global warming potential. CO₂e=carbon dioxide equivalents. *Best-case and worst-case scenarios.
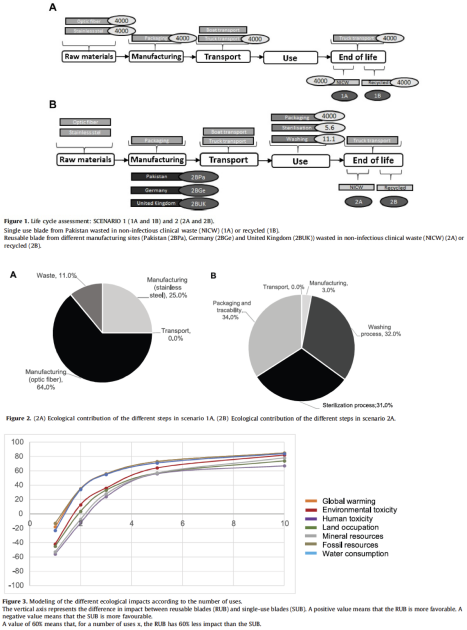
LCA is increasingly used to compare single-use versus reusable medical devices. Indeed, after several decades of widespread use of single-use medical devices, the issue of reuse has re-emerged in the public debate in recent years as ‘a solution to guarantee the safety of care in the face of shortages of medical devices, the challenges of scarcity of resources, the prohibitive carbon impact of drugs and medical devices and their purchase price’.
Por example, a team at Nîmes University Hospital has published a study describing a methodology using LCA to assess the transition from disposable laryngoscope blades (SUB) to reusable blades (RUB) and to analyse the ecological and economic impact of this change. In 2021, 17,200 intubations were performed, requiring around 147 RUB blades. The switch from SUB to RUB resulted in an annual saving of 26.5 tonnes of CO2eq (impact on global warming), equivalent to 120,000 km travelled by car. This has avoided the extraction of 6.6 tonnes of Oileq (oil) and 579 kg of copper (mineral resources) per year. This action has also reduced land use by 626 m² per year and saved 221.6 m³ of water per year. The average cost per intubation ranged from $3.16 [$3.15-3.16] for SUBs to $2.81 [$2.77-2.85] for RUBs, representing an average saving of $0.35 per intubation, or an annual saving of $5,783.50 [$5074.00-6192.00]. RUB blades are preferable from 3 and 86 uses respectively, from an ecological and economic point of view.