Dependence on fossil fuels: a challenge that goes beyond ecological impact
Energy consumption and greenhouse gas emissions: essential for good healthcare?
In order to provide appropriate medical care that meets patients' needs, the healthcare system requires energy and raw materials, which directly or indirectly translates into the consumption of material resources. Today, most of these resources are fossil fuels, since 80% of the primary energy consumed in the world is provided by the gas, coal and oil triad, while plastic consumables and a number of medicines are derived from the petrochemical industry. There therefore seems to be a correlation between sufficient access to these resources and the ability to provide medical treatment.
This raises two questions:
What is the nature of this correlation, and up to what level of resource consumption does it hold? In other words, is there a limit beyond which mobilising more fossil material resources can no longer improve the quality of care?
Is the performance of the healthcare system the only factor that determines the health of populations?
In an attempt to provide some answers, it is interesting to analyse the two graphs below, the key points of which have been summarised in the accompanying table.
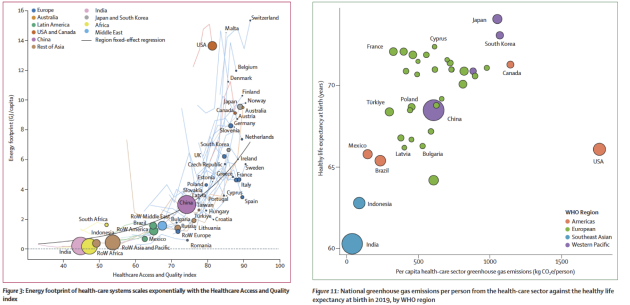
The first graph illustrates the relationship between 1) the energy footprint of the healthcare system (in GJ/capita) and 2) a healthcare system performance indicator, the Health Care Access and Quality Index (which measures mortality rates for 32 causes preventable by effective medical care).
The second graph illustrates the relationship between 1) GHG emissions from the healthcare sector per capita (kgCO2/person) and life expectancy at birth (in years).
It is essential to understand that our healthcare system is heavily dependent on fossil fuels. Studies show a correlation between the quality of care (measured by the Health Care Access and Quality Index) and energy consumption. The more energy a country consumes, the better the quality of care. However, some countries, such as Spain, manage to provide quality care with lower energy consumption, while others, such as the United States, consume much more for similar or inferior results.
Figure de gauche : Lines represent the evolution for years 1995, 2000, 2005, 2010, and 2015. Dots are proportional to the populations in 2015. The black line represents the regression with country fixed effects (table). Luxembourg is an outlier and has therefore not been shown (appendix p 14). For Canada, Switzerland, Finland, Malta, Norway, Netherlands, Slovenia, Slovakia, United States and Taiwan, data has been smoothed across 3 years to avoid sawtooths that did not reflect real dynamics (the maximum difference between the smoothed and unsmoothed data was of 24%). RoW=rest of the world.
Figure de droite : The point circle size is proportional to country population. kgCO2e=kilograms of carbon dioxide equivalent.
A number of points can be made from an analysis of the data:
Link between energy consumption and healthcare system performance: There is a correlation between the amount of energy consumed by the healthcare system and its performance. This link seems to follow an exponential trend. However, some countries, such as Spain, manage to achieve a very high level of performance (measured by the HAQ) while at the same time optimising their energy consumption, i.e. staying below the black curve in the graph on the left. Conversely, countries such as the United States achieve a lower level of performance while consuming more energy, putting them above this curve.
Life expectancy and carbon footprint: Life expectancy at birth also shows a correlation with the carbon footprint of the healthcare system, as shown in the graph to the right. However, this correlation is not linear. For example, the United States has a healthcare system with a high carbon footprint, but life expectancy remains relatively low.
Other factors influencing health: By comparing two countries such as Canada and Japan, which have similar indicators of healthcare system performance (HAQ), energy consumption and carbon footprint, but very different healthy life expectancies, we can conclude that there are other factors influencing health than just healthcare system performance.
In conclusion, there are two key messages here:
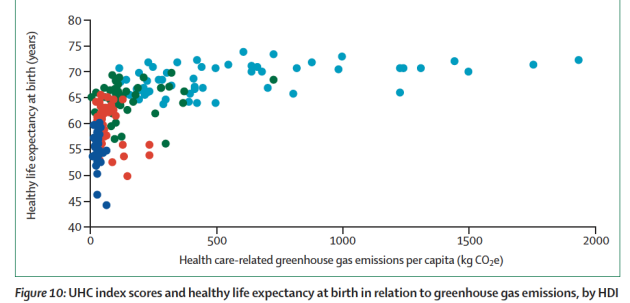
Higher greenhouse gas emissions from the healthcare system are correlated with longer healthy life expectancy at birth, up to around 400 kg of CO2e per capita. Above this threshold, healthy life expectancy at birth is decoupled from the carbon footprint of the healthcare system. This highlights that it is possible to offer accessible quality care without the need for high carbon intensity above this threshold. This means that up to a certain level of CO2 emissions, there appears to be a link between emissions and better general health, but after that point there is no further improvement, and it is entirely possible to maintain quality healthcare without increasing carbon emissions.
National per-capita greenhouse gas emissions from the health-care sector in 2021 versus healthy life expectancy at birth in 2019 (bottom; countries without an HDI score are not included because they do not have values for healthy life expectancy at birth); six countries with extreme values (>2000 kg CO2e) were excluded. CO2e=CO2 equivalent. HDI=Human Development Index. NA=not available. UHC=universal health coverage
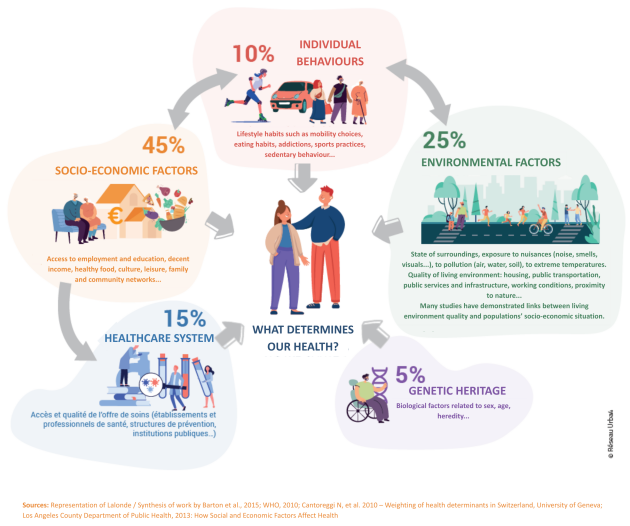
In public health, a health determinant is a factor that influences the state of health of an individual or a population, either alone or in combination with other factors. These determinants can be classified into different categories, and each can affect an individual's health in a different way. Researchers estimate that socio-economic and environmental factors account for around 70% of our state of health. This shows that our health depends above all on our environment, whether physical, social or economic, and goes far beyond the healthcare system or exemplary individual behaviour. This is why public action, by modifying the environment, the living environment and the habits of individuals, plays a key role in creating an environment conducive to health.
Fairness and sustainability: two irreconcilable objectives at the present time
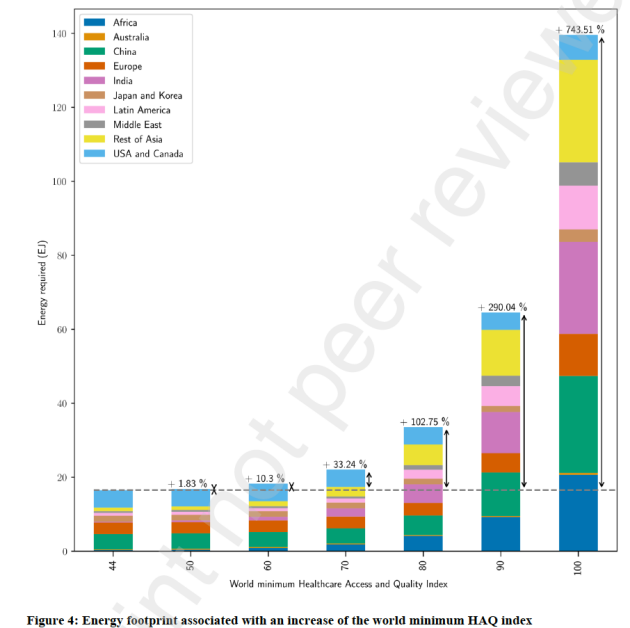
Increasing the global minimum HAQ index from 44 to 70 increases the energy footprint of healthcare by 33%, while increasing it to 90 or 100 increases it by 290% and 744% respectively (see graph below). This phenomenon can be explained by the exponential nature of the relationship between energy and the HAQ index, as well as by the fact that a higher minimum index concerns a growing number of people, which increases the demand for energy. In other words, increasing the HAQ index requires a much greater amount of energy as the index approaches higher values. This also demonstrates that an improvement in health affects a growing number of people, which multiplies the impact on the energy used for healthcare.
This observation underlines the fact that, as healthcare systems currently stand, it is neither conceivable nor materially possible to guarantee universal access to a high-performance healthcare system for all without exponentially increasing the consumption of energy resources and, consequently, the associated environmental impacts. All other things being equal, it seems that equity and sustainability are incompatible in this model. It therefore seems imperative to rethink the organisation of healthcare systems in order to reconcile universal healthcare coverage, fair care and limiting the environmental impact of the healthcare system (inputs and pollution).
In 2015, the minimum HAQ index was 44. Bars above the horizontal gray line represent the energy necessary to increase every region to a higher minimum HAQ index according to the regression of figure 3.
Dependence on fossil fuels: a question of resilience
Dependence on fossil fuels also raises issues of resilience and sovereignty, particularly with regard to the ability of governments to guarantee continuity of care in a sector that is dependent on fossil fuels and their imports.
Most European countries, including France, are almost 100% dependent on fossil fuel imports. What's more, some regions have surprising levels of import dependency. For example, although the Middle East produces 74 million tonnes of fossil fuels for its healthcare systems and consumes only 9 million tonnes, it remains 67% dependent on fossil fuel imports. This dependence stems from the fossil fuels present in the imported goods. For example, if the Middle East imports medicines from the United States, these medicines may have been manufactured using fossil fuels that do not originate in the Middle East.
This situation raises two major issues:
Climate change requires us to drastically limit our extraction and combustion of fossil fuels. If this transition is not chosen and organised, it will inevitably be suffered, because these resources (on a human timescale) are non-renewable. What's more, certain production peaks, such as that for conventional oil, have already been exceeded, and others will be reached in the decades to come. It is therefore not rational for the healthcare sector to continue to depend on a resource whose long-term availability must (and will) decline.
Export-dependent countries are the most vulnerable in this context, as they will be the first to suffer the consequences of the increasing scarcity of resources, whether they choose to or are forced to do so. It is therefore becoming imperative to build resilient, sober healthcare systems that are free from fossil fuel constraints. This requires a long-term strategy of bifurcation, anticipated and planned over several decades, to prevent shortages and guarantee continuity of care for patients.